Abstract

Introduction: Hemophilia, an inherited bleeding disorder leading to deficiency of clotting factor VIII (hemophilia A) or factor IX (hemophilia B), affects approximately 30,000 people in the United States. Widespread availability of factor replacement products led to reductions in bleeding complications, but contamination of the blood supply prior to implementation of mitigation measures led to increased rates of chronic viral infections among persons with hemophilia (PWH). However, mortality rates among PWH have not been systematically evaluated in a decade. Evaluation of mortality rates helps quantify the burden of hemophilia and helps identify trends, should they exist.
Methods: Deaths among PWH in the United States were identified through mortality reporting to bleeding disorder surveillance programs. Deaths occurring 2000-2011 were reported to the Universal Data Collection (UDC) system, a collaboration with the Centers for Disease Control and Prevention (CDC) and the U.S. Hemophilia Treatment Center Network (USHTCN). Deaths occurring during 2012-2021 were reported to the Community Counts (CC) system, a collaboration between CDC, the American Thrombosis and Hemostasis Network (ATHN), and the USHTCN. Deaths were reported using standardized mortality forms. The total population under study was estimated using information from the CC HTC Population Profile, an annual census of the Hemophilia Treatment Center (HTC) patient populations, and UDC Registration records. Data collection included patient demography and disease characteristics. Mortality rates, adjusted for age, severity, and race/ethnicity, were estimated, assuming a Poisson distribution. Trends over time were assessed by including time period in the model. Non-overlapping confidence intervals and p for trend < 0.05 were considered statistically significant.
Results: For the time period 2000-2021 1,673 deaths among PWH A and 401 deaths among PWH B were reported from participating HTCs in the United States. Of these, over 97% were male, 1,649 hemophilia A and 349 hemophilia B. Thus, stratum-specific mortality rates were only calculable among males with hemophilia A (MWH-A) or hemophilia B (MWH-B). For both MWH-A and MWH-B mortality rates were highest among the oldest age groups across all time periods.
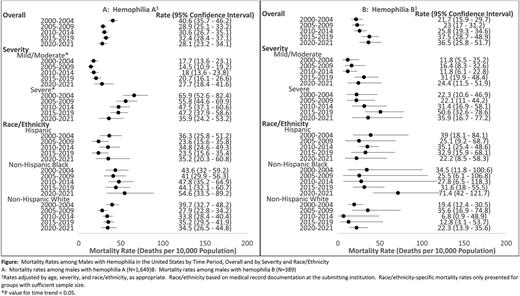
Mortality rates among MWH-A decreased after the 2000-2004 period but remained stable thereafter, with the mortality rate during the 2020-2021 period being 28.1 (95% Confidence Interval [CI]: 23.2 - 34.1) deaths per 10,000 population (Panel A). While confidence intervals overlapped, mortality rate estimates among MWH-A with mild or moderate disease generally rose over each time period and the trend was statistically significant (p < 0.05). In 2020-2021, the mortality rate among MWH-A with mild or moderate disease was 27.7 (95% CI: 18.4 - 41.6) deaths per 10,000 population. In contrast, mortality rate estimates among MWH-A with severe disease declined over each time period; while confidence intervals overlapped, the trend was significant (p < 0.05). In 2020-2021, the mortality rate among MWH-A with severe disease was 35.9 (95% CI: 24.2 - 53.2) deaths per 10,000 population. There were no clear temporal mortality trends among Hispanic, non-Hispanic Black, or non-Hispanic White MWH-A.
Mortality rates among MWH-B remained relatively stable across all time periods, with confidence intervals overlapping; the mortality rate among MWH-B was similar to that among MWH-A in the 2020-2021 period (36.5 [95% CI: 25.8 - 51.7] deaths per 10,000 population) (Panel B). Severity-specific and race/ethnicity-specific mortality rate estimates among MWH-B were similar across all time periods, but the analysis was underpowered. Of note, the mortality rate among non-Hispanic Black MWH-B was significantly higher than that among non-Hispanic White MWH-B during the 2020-2021 period (71.4 [95% CI: 42.0 - 121.7] and 22.3 [95% CI: 13.9 - 35.6], respectively).
Conclusions: This assessment of mortality rates among PWH using national data indicates there have been improvements in mortality rates among MWH-A, but this improvement may be limited to males with severe disease. Limitations related to estimate precision preclude the assessment of trends in mortality rates among MWH-B and among females with hemophilia.
Disclosures
Sharathkumar:University of Iowa Clinical Committee: Membership on an entity's Board of Directors or advisory committees; University of Iowa: Current Employment; Amgen, CDC/ATHN/HRSA: Research Funding; Genentech, Takeda, CSL: Honoraria. Croteau:Spark Therapeutics, Genentech, Sanofi: Research Funding; Bayer, Pfizer: Honoraria; ATHN, Hemophilia Alliance, THSNA: Membership on an entity's Board of Directors or advisory committees; Bayer, Pfizer, Sanofi, BioMarin, HemaBiologics: Consultancy. Pruthi:CSL Behring: Honoraria, Membership on an entity's Board of Directors or advisory committees; Genentech Inc: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bayer Healthcare AG: Honoraria, Membership on an entity's Board of Directors or advisory committees; HEMA Biologics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Instrumentation Laboratory: Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy. Peltier:Novo Nordisk: Consultancy, Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal